Did it work the way we hoped it would?
When designing a new service, it is crucial that we fully evaluate it so we can understand if it produced the outcomes desired, and to what extent. We carried out a mixed methods service evaluation for the first year of Connecting Care for Care with a particular focus on our specialist outreach multidisciplinary teams (MDTs) and clinics.
Measures
Our outcome measures covered all aspects of the potential impact:
- the service – number of cases discussed or seen in the MDT meeting and the resultant impact on secondary care usage from hospital episode data
- the service users – patient reported experience measures (PREMs)
- the professionals – participant feedback questionnaires from those attending MDTs and clinics
Results
The service: in the initial 12 months of the pilot, 24 MDT meetings and clinics took place. Seven to 15 professionals attended each MDT meeting and 154 cases were discussed. 126 patients were seen in the clinics. Outcomes of the meeting or clinic were categorised:
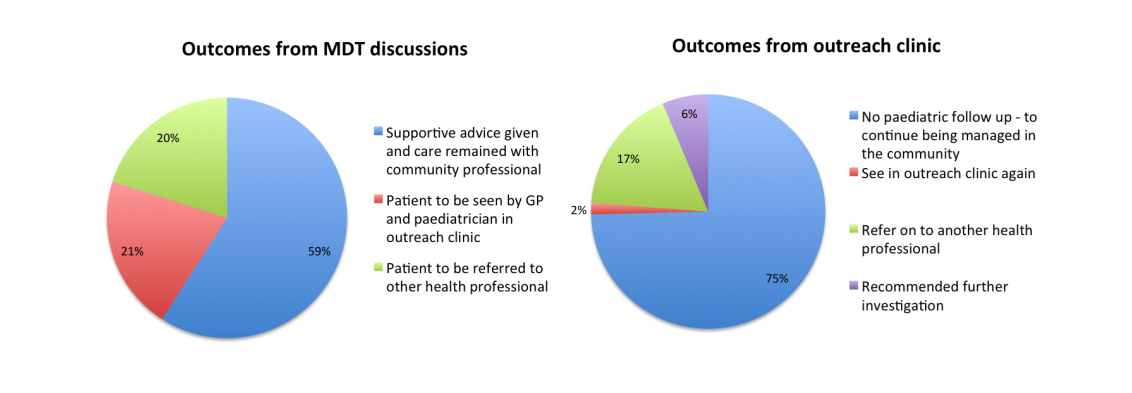
We then looked at what impact this had on secondary care usage. In one hub, 39 per cent of new patient hospital appointments were avoided altogether and a further 42 per cent of appointments were shifted from hospital to GP practice. In addition, there was a 19 per cent decrease in sub-specialty referrals, a 17 per cent reduction in admissions and a 10 per cent decrease in A&E attenders. Smaller hubs running at lower capacity in early stages of implementation had less impact on hospital activity. The table below summarises the data.
|
|
Non-hub practices |
Hub 1 (multi-practice hub) |
Hub 2 (single-practice hub) |
Hub 3 (single-practice hub) |
|
New general paediatric outpatient appointments
|
23% ↑ |
134 to 25 81% ↓ [39% avoided, 42% shifted to out of hospital] |
54 to 20 63% ↓ [All 63% shifted to out of hospital] |
28 to 10 64% ↓ [All 64% shifted to out of hospital] |
|
New sub-specialty paediatric hospital outpatient appointments |
5% ↑ |
180 to 146 19% ↓ |
64 to 44 31% ↓ |
34 to 29 15% ↓ |
|
Paediatric A&E attendances |
12% ↓ |
1613 to 1263 22% ↓ |
520 to 541 4% ↑ |
304 to 215 29% ↓ |
|
Patients who attend paediatric A&E greater than four times a year |
48% ↑ |
69 to 47 32% ↓ |
27 to 39 44% ↑ |
5 to 5
|
|
General paediatric admissions into hospital |
13% ↓
|
221 to 183 17% ↓ |
109 to 91 17% ↓ |
37 to 35 5% ↓ |
The patients: patients preferred appointments at the GP practice, gained increased confidence in taking their child to the GP and all respondents said they would recommend the service to family and friends.
The professionals: 50 professionals who had attended the child health GP hubs over the first 12 months of the pilot were contacted by email asking for feedback. Participants ‘agreed’ or ‘strongly agreed’ that the hubs had helped them to: gain knowledge of local services; improve collaboration and professional relationships; and increase professional capability, with the exception of three neutral responses regarding professional capability. Interestingly, the development of social capital, which we define as ‘trust, reciprocity and collaboration’ was the benefit most strongly identified by participants (82 per cent ‘strongly agreed’).
Conclusions
We were really encouraged by our evaluation findings. We found that child health GP hubs, designed to increase the connections between secondary and primary care, are effective in reducing secondary care usage, with high patient satisfaction ratings whilst providing learning for professionals and developing social capital.
The child health GP hubs continue to expand their pilot phase in north west London and the breadth of professionals involved in the hub MDTs continues to increase. The hubs also provide an important mechanism for the training of the future child health workforce. If we are to successfully change the way in which care is delivered, education and workforce development need to be at the heart of all service innovations like these.